Healthcare in the age of AI: How will artificial intelligence impact future decision-making?
Authored by: Tom Donnelly, Constanza Salas, Jhon Galindo and Rachel Howard
Artificial Intelligence (AI) has recently surged in popularity, thanks in part to innovations like ChatGPT, which represents a significant step towards generating human-like text from simple prompts. In the healthcare sector, AI’s advancement has begun to impact prescribing, particularly in addressing the growing challenge of antimicrobial resistance. A pivotal study in 2023 has revealed that an AI model produced better therapeutic outcomes than prescriptions written by doctors.
However, AI models such as ChatGPT have their limitations, including deficiencies in mathematical capabilities and a restricted knowledge scope, limited to data available up to 2021. Furthermore, they carry a substantial risk of generating false information. This raises a fundamental question: where does AI acquire its learning? A 2023 Pew Research study has highlighted the concerns of many U.S. patients regarding AI-driven robots in surgical procedures and the security of AI in managing health records. Given these current apprehensions surrounding AI, researchers have emphasized the critical need to combine AI with human expertise.
To navigate through these complexities, we have been investigating how AI is transforming the prescribing process and its impact on patient outcomes and healthcare costs. To achieve this, we recently collaborated with Medefield to conduct a survey involving 177 general practitioners (GPs) across the United States, France, Germany, Spain, and the United Kingdom. Additionally, we surveyed 14 payers from Research Partnership’s global payer network in France, Germany, Italy, Spain, and the UK.
Current AI usage, perceptions, and prospects of AI adoption
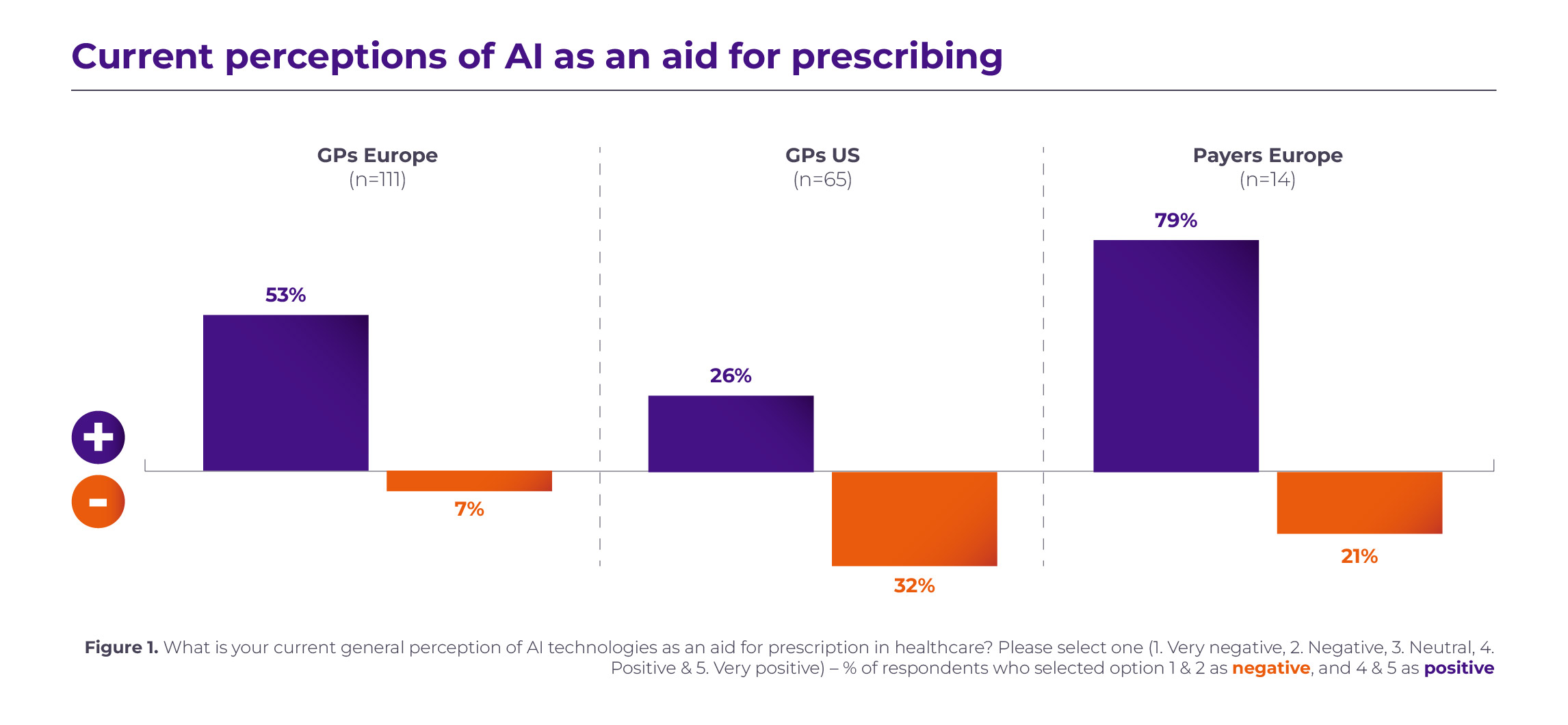
Our findings reveal that in Europe, 40% of GPs have never utilized AI tools to assist in their prescribing practices. In the U.S., the adoption of AI is even lower, with 60% of GPs not using AI at all. Moreover, their perceptions of AI’s role in supporting prescription practices vary significantly, with European GPs generally holding a more favorable view compared to their U.S. counterparts. Conversely, European payers hold even more positive perceptions than both European and U.S. GPs (see Figure 1).
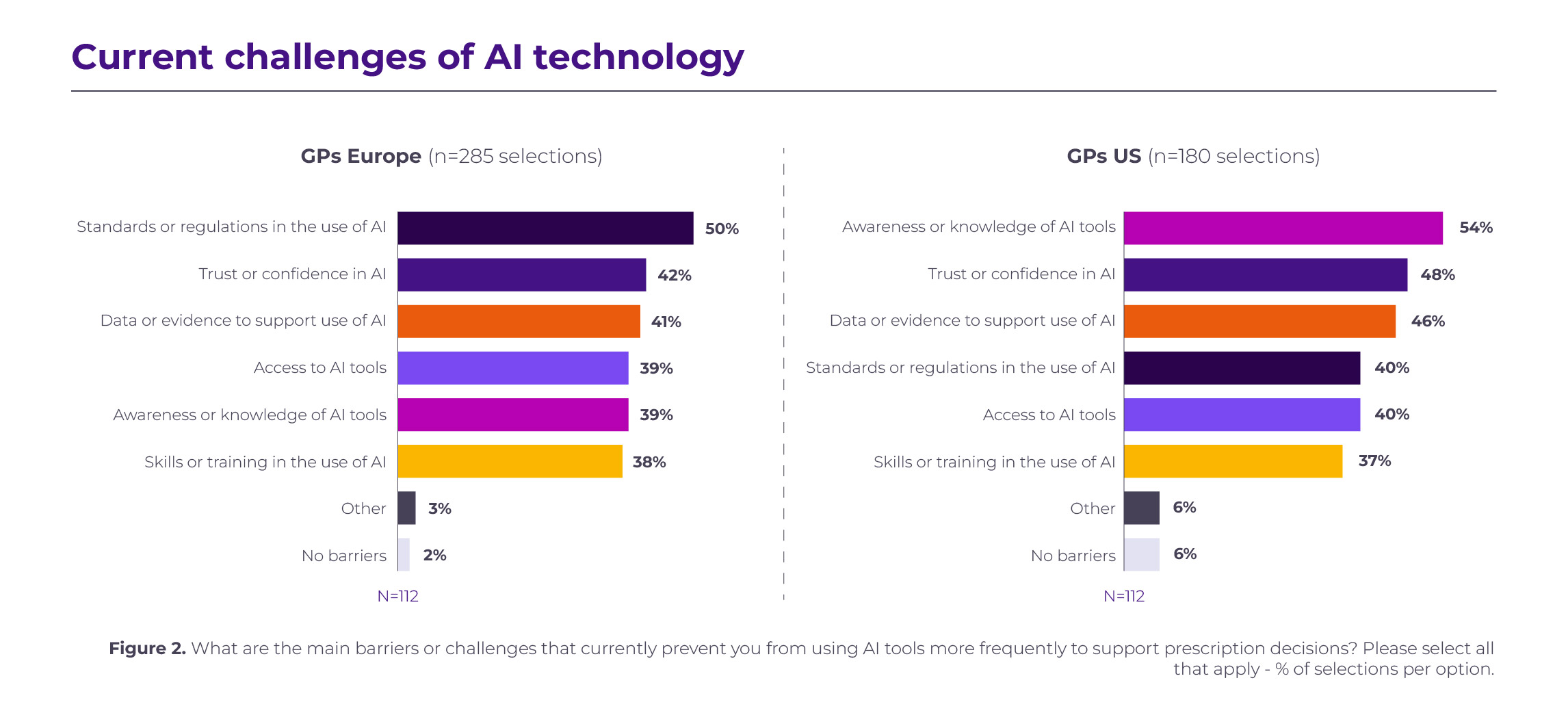
 To understand the underlying reasons for these perceptions, we delved into the primary challenges that GPs believe hinder the increased use of AI. In Europe, half of the GPs mentioned “standards or regulations in the use of AI” as their main challenge, while GPs in the U.S. identified a different obstacle, with over half of them indicating a lack of “awareness or knowledge of AI tools” as a major factor (see Figure 2).
To understand the underlying reasons for these perceptions, we delved into the primary challenges that GPs believe hinder the increased use of AI. In Europe, half of the GPs mentioned “standards or regulations in the use of AI” as their main challenge, while GPs in the U.S. identified a different obstacle, with over half of them indicating a lack of “awareness or knowledge of AI tools” as a major factor (see Figure 2).
 Having examined the current usage, perceptions, and obstacles surrounding the utilization of AI in prescription practices, we questioned our respondents about the future prospects of AI adoption in their field over the next 5 years. Remarkably, 62% of European GPs expressed their willingness to increase their use of AI in the prescription process, while in the U.S., only 49% of GPs shared a similar inclination.
Having examined the current usage, perceptions, and obstacles surrounding the utilization of AI in prescription practices, we questioned our respondents about the future prospects of AI adoption in their field over the next 5 years. Remarkably, 62% of European GPs expressed their willingness to increase their use of AI in the prescription process, while in the U.S., only 49% of GPs shared a similar inclination.
Future impact of AI on patient outcomes
Shifting our focus to the future impact of AI on patient outcomes in the next 5 years, we found that European GPs tend to hold a more positive view, while their US counterparts were slightly less optimistic (Figure 3). 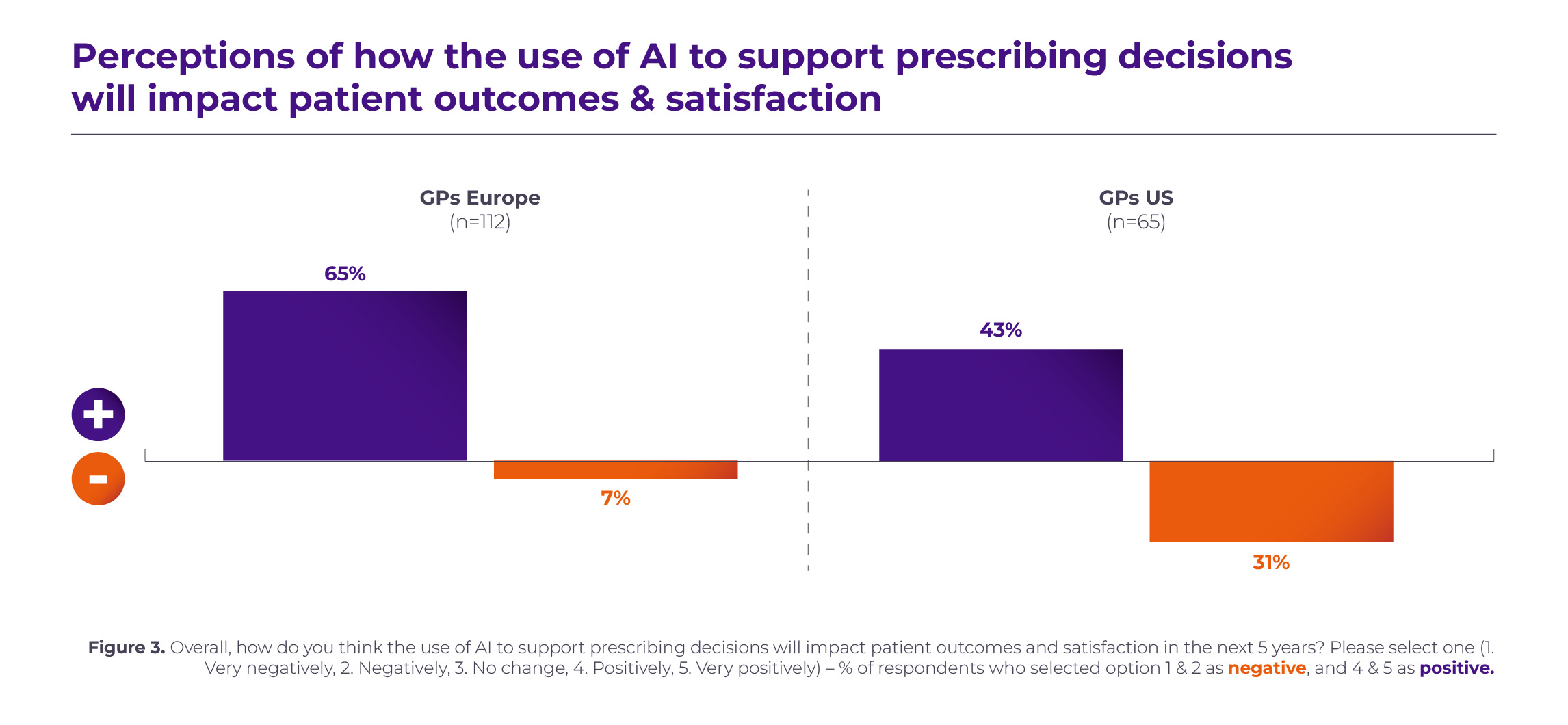
In alignment with current AI perceptions, European payers tend to be the most optimistic about AI’s impact on patient outcomes over the next 5 years. Over 70% of payers expressed a positive perception of how the use of AI to support prescription decisions will enhance the quality of care and patient outcomes. An analysis of the rationale provided by payers is presented below (see Figure 4).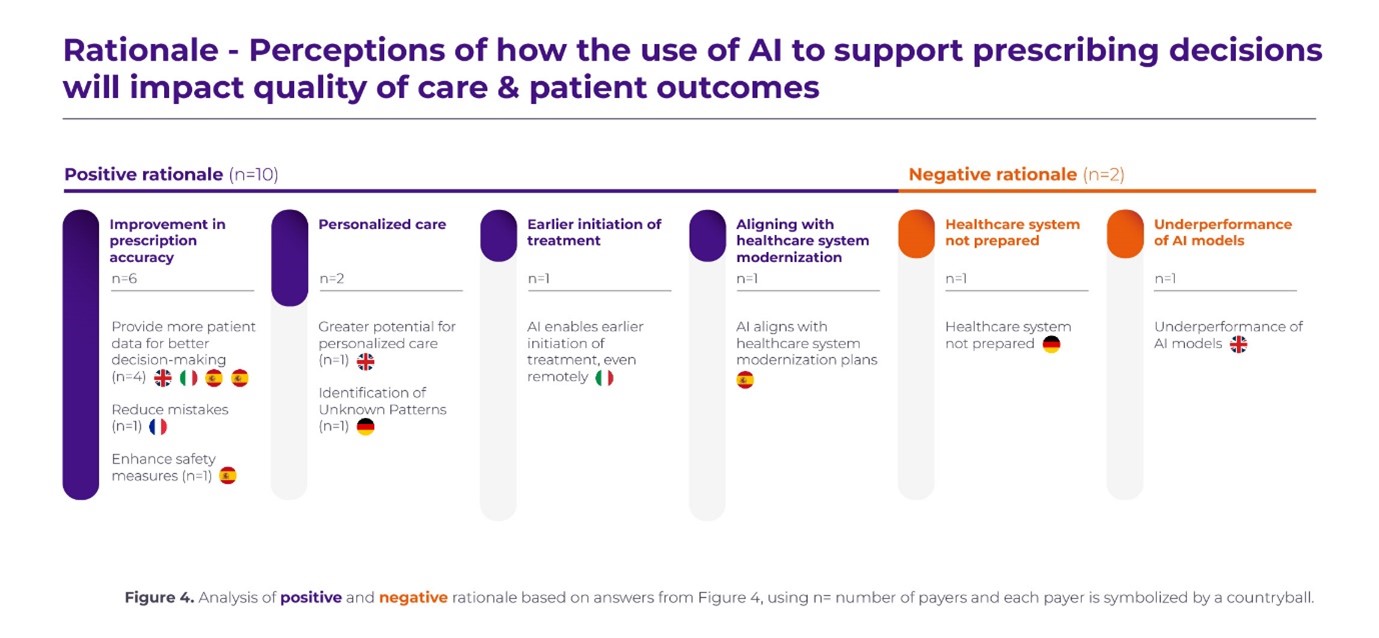
Future impact of AI on healthcare costs and market access
Regarding the impact of AI on healthcare costs, 43% of European payers anticipate that AI technologies will decrease healthcare costs within the next 5 years. Italy exhibits notably positive expectations, followed by France, while other countries hold more mixed views. Those who believe that AI will reduce healthcare costs anticipate savings through improved efficiency, including the reduction of unnecessary steps, better patient data management, and avoidance of expenditures related to inappropriate treatment. One payer, based in the UK, noted that they are “less likely to provide treatments with little or no efficacy using historical data [with the use of AI], thus avoiding expenditures related to inappropriate treatment.”
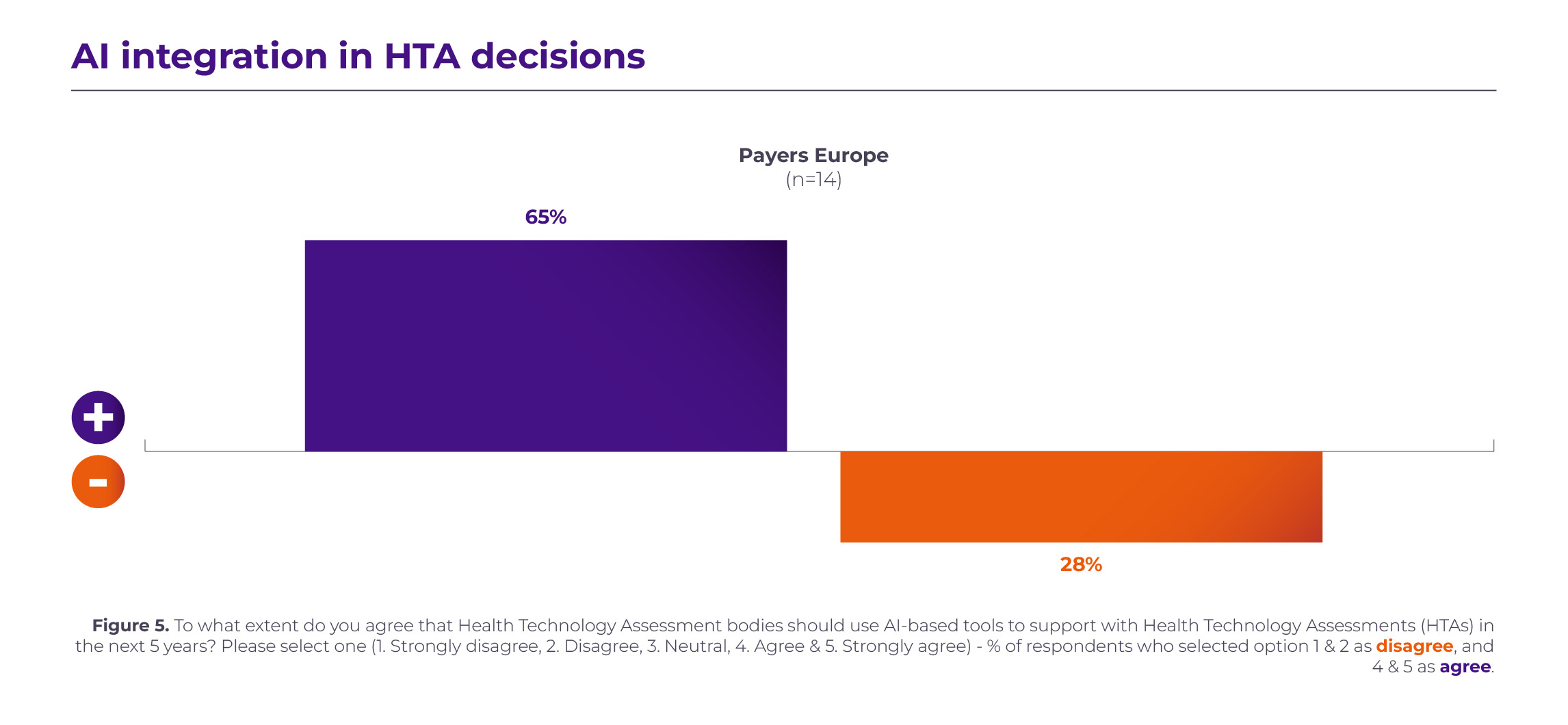
Overall, payers tend to agree that AI has the potential to support health technology assessment (HTA) evaluations in the next 5 years (see Figure 5). Some of the reasons given for this positive perspective include faster clinical trial and Real-World Data analyses or providing further evidence for HTA decisions and support with routine tasks. Nevertheless, certain payers, particularly those in Germany, maintain a more negative view, primarily due to the need for human oversight, lack of current use or evidence, and concerns about bias in the AI models. A German payer commented, “The issue lies in AI models that have potentially been trained with biases.”
 We gathered concluding thoughts from our surveyed payers. Some believe that collaborating on AI algorithms is more reliable than human analysis. For example, an Italian payer noted that “[AI] might be helpful, but the final decision should always be made by humans. It is important to establish laws and specific legislation regarding the proper use of AI to protect data and privacy.” Others contend that humans will always have the final say, emphasizing the necessity of data protection legislation for AI use. A Spanish payer expressed the belief that “AI has great potential, offering benefits such as increased accuracy and speed, reduced costs and human errors, and improved access to healthcare in remote areas.”
We gathered concluding thoughts from our surveyed payers. Some believe that collaborating on AI algorithms is more reliable than human analysis. For example, an Italian payer noted that “[AI] might be helpful, but the final decision should always be made by humans. It is important to establish laws and specific legislation regarding the proper use of AI to protect data and privacy.” Others contend that humans will always have the final say, emphasizing the necessity of data protection legislation for AI use. A Spanish payer expressed the belief that “AI has great potential, offering benefits such as increased accuracy and speed, reduced costs and human errors, and improved access to healthcare in remote areas.”
Work to be done
Our research revealed that US GPs are currently less open to AI-aided prescribing than their European counterparts. This reflects a lower experience level with these tools to date and aligns with US patient concerns outlined in other literature. European payers showed more optimism about the use of AI for this purpose.
There is recognition among both GPs and payers that adopting AI in prescribing can improve patient outcomes, increase patient satisfaction, and from the payer perspective ultimately translate to cost savings. However, some point out that for these benefits to be realised, there is work to be done in preparing healthcare systems to effectively adopt these tools. In particular, concerns relating to awareness, regulations, data protection, and bias need to be addressed to fully embrace AI. Ultimately, even if AI can ultimately realize its immense potential within healthcare, there is a consensus that human checking will still be required.
In conclusion, the rapid advancement of AI, exemplified by innovations like ChatGPT, is reshaping the landscape of healthcare and prescription practices. While AI holds great promise in improving therapeutic outcomes and potentially reducing healthcare costs, our research underscores the need for a thoughtful and measured approach.
As we navigate through the evolving relationship between AI and healthcare, it is essential to address the challenges that currently hinder its widespread adoption. These include the need for standardized regulations, increased awareness and knowledge among healthcare practitioners, and vigilant efforts to mitigate biases in AI models. Moreover, the human element remains indispensable in healthcare decision-making, with AI serving as a valuable tool rather than a replacement.
The divergent perceptions of AI’s role and impact among healthcare professionals across different regions underline the importance of a nuanced and region-specific strategy for AI integration. European and U.S. healthcare stakeholders have their unique perspectives and concerns, necessitating tailored approaches to maximize AI’s benefits while minimizing its risks.
In this dynamic landscape, it is crucial to strike a balance between AI’s capabilities and human expertise. The collaboration between technology and healthcare professionals, along with the development of robust regulatory frameworks, will be pivotal in harnessing AI’s full potential for the betterment of patient outcomes, cost-effective healthcare, and the advancement of the healthcare industry as a whole.
In the coming years, as AI continues to evolve and healthcare systems adapt, our collective efforts to bridge the gap between AI’s promise and practical implementation will play a decisive role in shaping the future of healthcare. The path forward may be challenging, but it is one that holds the promise of more efficient, effective, and accessible healthcare for all.
References available upon request.

Other insights.
Jump to a slide with the slide dots.
A common reality: How augmented reality is transforming the future of pharmaceutical marketing
Harrison Gaiger explores the ways in which AR is transforming the future of pharmaceutical marketing.
Read moreAI: Powering healthcare, empowering patients
In the face of the coronavirus, innovative technologies such as artificial intelligence (AI) and machine learning (ML) have proven vital.
Read moreSign up to receive Rapport.
Rapport is our monthly newsletter where we share our latest expertise and experience.