We recently ran a webinar called RP Investigates, where Head of Living With, Mariel Metcalfe talked to a patient about the challenges of living with the disease. In this follow-up article, Head of Therapy Watch, Helen Parfitt and Mariel Metcalfe, investigate lupus from the perspective of both healthcare professionals (HCPs) and patients using data from our syndicated research studies Therapy Watch and Living With.
Lupus is a complex, chronic, unpredictable and often invisible autoimmune disease that can severely disrupt patients’ lives and negatively impacts quality of life. Lupus is thought to affect at least five million people worldwide, with around 16,000 new cases each year in the US alone. Prevalence is highest amongst women of childbearing age, and some ethnic or racial groups are not only more likely to develop lupus but then face higher rates of morbidity and mortality when they do so. The potential root causes of lupus are also diverse, ranging from hormonal to genetic to environmental.
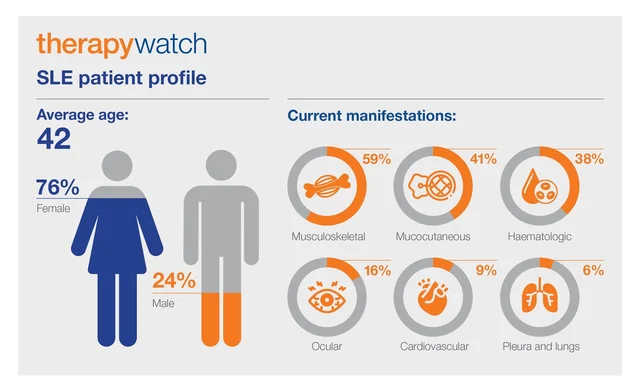
Lupus symptoms can extend from mild to life-threatening. Among the most commonly reported are joint or muscle pain, fatigue, skin rashes, fever, nausea and depression. US data from our global Therapy Watch tracker showed that 9 out of 10 patients have at least one symptom as a result of systemic lupus erythematosus (SLE) or associated lupus nephritis (LN).
At its worst, lupus can lead to potentially fatal complications such as kidney failure, cardiovascular disease or stroke, yet diagnosing lupus can be challenging. The classic symptoms overlap with those of many other diseases, symptoms come and go in a pattern of flare and remission, and the number and type of symptoms vary from one person to the next.
“It was scary, caused me to have a lot of questions. Am I going to die? Is this curable? What can I do? Where did I get it? Why do I have it?” Female, 51, SLE
The Therapy Watch data showed that 78% of SLE patients and 84% of LN patients have comorbid conditions. The main comorbidities across both groups are high blood pressure and anaemia, with prevalence increasing among LN patients.
Diagnosing and living with lupus
Not knowing when and why lupus may ‘flare up’, both complicates initial diagnosis and leaves patients living with uncertainty. The awareness that multiple symptoms may turn up at any time causes stress and anxiety, which in themselves are further catalysts for flares.
Most lupus patients experience symptoms daily and over half of all patients interviewed for our Living with Lupus US 2021 report were currently experiencing a flare. This has a significant impact on patients’ daily activities, such as ability to exercise or socialise, and on their libido. The relative invisibility of lupus means patients’ symptoms are often not taken seriously by their friends, family or work colleagues.
“They say ‘Well, can you give us a few days’ notice before you get sick?’. I just wish there was more education and more advocacy for people like me because if you were a person in a wheelchair there are laws, right? But when I say I need something they act like I want special treatment.”
Female, 46, LN
It does not help that diagnosis often comes late or the disease is simply overlooked. Our Living With insights showed that most patients present to a HCP within around six months of onset. The diagnosis pathway is highly variable, though, and more than half of all patients are initially misdiagnosed. Patients’ emotions at the time of diagnosis reflect this uncertainty and the lack of understanding around the disease. Lupus patients tend to feel overwhelmed and anxious, although some are relieved that they at last have a confirmed diagnosis.
The treatment journey and management by HCPs
The treatment journey for lupus, including interactions with specific HCPs and prescribed lupus treatments, depends on the nature of the condition and its severity. Therapy Watch data indicated that the primary treaters for SLE are rheumatologists, while for LN both rheumatologists and nephrologists perform that function.
Treatment options for lupus typically include non-steroidal anti-inflammatory drugs (NSAIDs), anti-inflammatories such as corticosteroids, repurposed antimalarial therapies and immunosuppressants. New and emerging biological therapies, such as monoclonal antibodies, target B cells to prevent them from initiating the autoimmune process. Therapy Watch research found that 42% of SLE patients are currently taking steroids, while in LN patients’ steroid usage rises to 62%. According to our Living With Lupus insights, more than half of the patients interviewed were currently on steroids, and said they wanted to use them less.
In terms of shared management, SLE patients are more likely to be co-managed by their primary-care physicians (PCPs) alongside their specialist. LN patients tend to be jointly managed more commonly by rheumatologists and nephrologists. At the same time, LN patients seen by a nephrologist report less co-management overall. With SLE, nephrologists get more involved in disease management as the condition gets worse. LN patients find that PCPs or rheumatologists take on more of a role as the disease increases in severity. Treatment strategies tend to evolve in parallel.
In SLE patients, for example, therapies aimed at depleting B-cells are increasingly used as the disease gets worse. In LN, though, B-cell depleter use increases only marginally with disease severity (in around one in three patients), whereas MMF (Mycophenolate Mofetil) use and disease severity are more closely linked.
Monitoring and managing lupus
Clinicians use a variety of tools to monitor disease status and management. With SLE, these tools include biomarker testing, physician assessment, patient feedback and formal disease-activity tools. Similar tools are applied in managing LN, albeit with greater reliance on biomarker testing.
The physician-patient relationship is geared towards shared responsibility, as patients look for the knowledge and understanding to cope with a condition that affects everything they do. As most people with lupus are still relatively young, they have grown up in an Internet age, so have more awareness and confidence to interrogate information sources outside the traditional doctor-patient relationship. Our Living With research found that lupus patients generally have a good relationship with their HCP and are confident talking to these professionals about their condition. Patients feel their concerns are taken seriously and they trust HCPs completely in relation to their lupus.
All the same, there are communication gaps. Patients say they are given limited information at diagnosis, which leads many of them to seek information on lupus proactively outside HCP appointments. We found that patients want more insights into disease progression and greater access to online resources at diagnosis.
“I try to stay up-to-date on treatments and general information about the different diseases that I have, just so I can understand things as they happen.” Male, 51, SLE
The Living With research revealed that most patients already search online for information about lupus. More than half of all patients were engaged with social media and/or online support groups. Patients like speaking to other people with lupus, so they can share experiences and know that they are not alone in having to deal constantly with the condition and its consequences.
What patients want from lupus treatment
As the Living With insights made clear, lupus patients want more out of their treatments, they are looking for therapies with few side effects that can reduce flares, inflammation and fatigue, as well as reduce the need for steroid usage. Patients worry about side-effects, such as immunosuppression and weight gain, and fewer than one in 10 patients feel their current treatment has significantly improved their day-to-day activities. Moreover, US patients are generally concerned about being able to afford treatments in the future.
The way forward with lupus management
There are a number of routes forward to address and reconcile concerns about sub-optimal management of lupus. In terms of treatment choice, the lack of truly innovative and effective options means HCPs select therapies principally on the basis of efficacy. As the Therapy Watch data indicated, prescribers usually switch between products because the current treatment is simply not working.
For their part, patients want treatments that can improve their ability to complete everyday activities, exercise and sleep. Our Living With research found that one in four patients were looking for more awareness and understanding from the public about what lupus is, why it so often falls below the radar, and how it fundamentally affects patients’ daily life, working life and those around them.
Part of the solution will require more investment into finding better, safer, more effective treatments that enable patients to minimize steroid usage and achieve lasting relief from persistent symptoms. In the end, the best therapy for people with lupus will be one that can improve their overall quality of life.
For more information about our syndicated research capabilities, please contact:
Andie Vinycomb
Senior Business Development Executive
contact@researchpartnership.com
RP Investigates: Live Q&A – Living with Lupus
Watch the webcast