With patient centricity and improved patient engagement a central mission for much of healthcare, we conducted a study in China to find out what a telemedicine service in ophthalmology would need to offer to stand out and improve the patient experience and outcomes.
The rise in telemedicine platforms
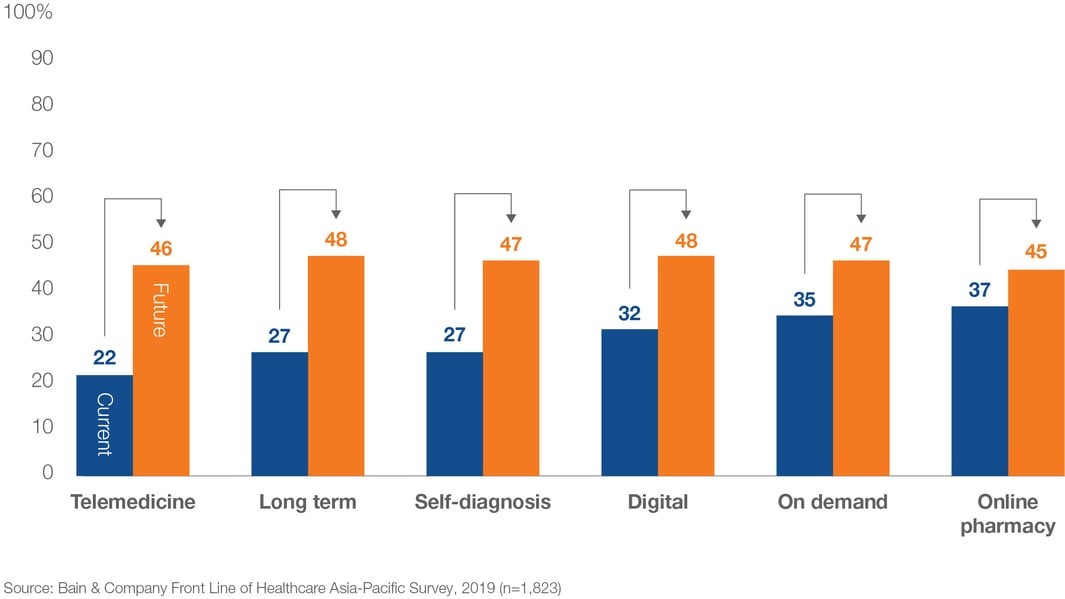
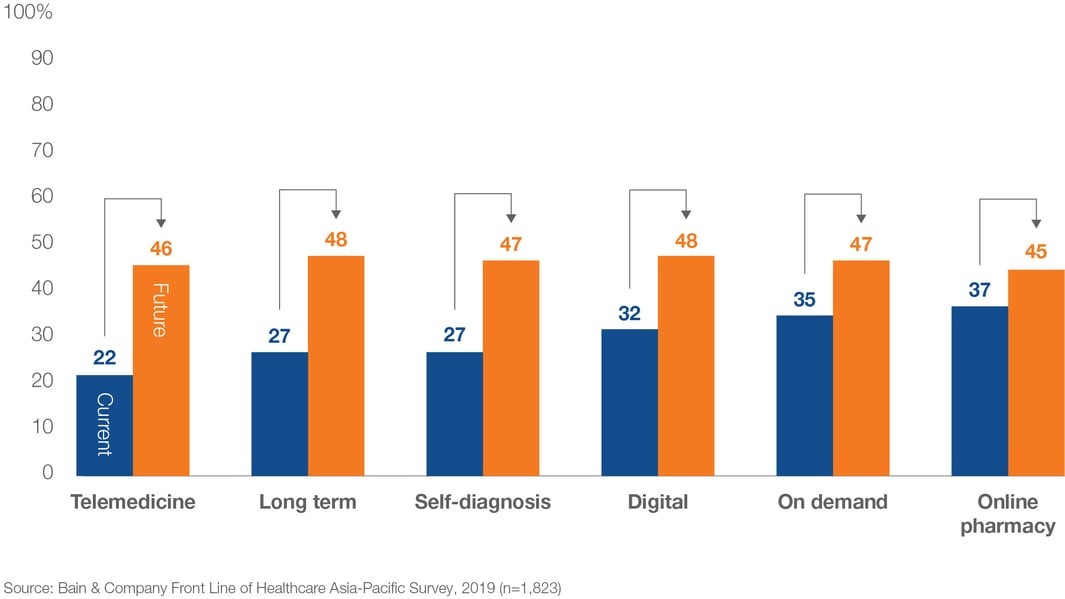
Telemedicine has disrupted the healthcare market worldwide and, since the pandemic, it is ubiquitous. Many countries in Asia have been at the forefront of using digital technologies in healthcare, and according to a survey by Bain & Company consumers in Asia-Pacific will increasingly adopt and use digital health tools over the next five years (see figure).
Some of the popular telemedicine platforms that have seen huge recent growth include Ping An Good Doctor (China), Halodoc (Indonesia) or Doctor Anywhere (across Vietnam, Malaysia, Thailand, Singapore, Philippines). These platforms offer a variety of services, from virtual consultations to booking home care services and online prescriptions. Uptake in Asia-Pacific has been helped by regulatory changes and the implementation of payment models. In Japan, for example, the government extended the use of telemedicine from follow-up visits only to initial consultations and the delivery of prescription drugs during the pandemic.
Improved access to care, convenience and anticipated time and cost efficiencies are some of the key end user benefits of telemedicine. But, with a multitude of telemedicine services competing for customers, how can a service provider ensure that their solution delivers these benefits and provides an outcome that is relevant for customers? Ultimately, a telemedicine tool needs to compete favorably and deliver at least equal satisfaction to in-person visits in order to attract customers.
Case study: Telemedicine users in China
To dig a little deeper into the user experience of telemedicine and evaluate what customers want from the service, we conducted a self-funded study in China where telemedicine has been broadly used for several years. We conducted web-assisted duos with retina specialists and ophthalmology patients, which included a mock patient-physician consultation using telemedicine to mimic the experience. Our findings revealed some interesting insights into what customers expect from a telemedicine service.
1. One-stop touchpoint for quick and easy access to care
One of the essential features of telemedicine is conducting consultations virtually, either by phone, video or text. Users also want quick and easy access to the service. In our study, patients reported using telemedicine for a triage of new symptoms, or in an emergency situation to allow quick assessment of their situation and advice on whether they needed to go to the hospital for further examination.
In China in particular, long travel and waiting times make access to Tier 3 hospitals challenging. Telemedicine enables patients to access specialists from the comfort of their own homes. Our respondents suggested that it would also allow them to seek out additional opinions, for example to confirm a diagnosis with a different physician or, if they are not satisfied with the care received in a community hospital, reach out to a more senior, experienced doctor.
However, respondents felt that telemedicine was not (yet) connecting the entire patient journey. Patients greatly desire a one-stop touchpoint from appointment booking to virtual consultations and prescriptions. Both physicians and patients suggested that in order for the tool to be most useful, it would need to include and provide access to a broad network of hospitals and physicians. Patients would ideally like to have ‘their’ physician included on the platform, which would allow continuity of care since some hospitals might not accept test results from other hospitals.
Respondents reported mixed experiences with online prescriptions. Physicians told us that they are often constrained by what medication a specific telemedicine service offers, meaning that the patient would need to come to the hospital to pick up the prescription, despite having had the virtual consultation. Respondents agreed that a full service enabling online prescriptions for repeat medication, as well as delivery to the patient, would be most convenient and patient friendly.
“At the moment the doctors can only give qualitative feedback over telemedicine, but if we want to be prescribed medication or prescribed a particular examination they can’t do that, we’ll still need to go to a hospital for a prescription. If they can prescribe me medicine through telemedicine and have it delivered to me that will be better.” (Ophthalmology patient, China)
2. Opportunity for follow-up monitoring but limited use for diagnostic consultations
In our research, we wanted to know where users felt telemedicine worked well and where it was lacking. It was perceived that telemedicine is most suitable for follow-up/ monitoring consultations after a clear diagnosis has already been reached. Telemedicine, in this instance, was considered to be cost saving and time efficient for patients and physicians.
A few retina specialists highlighted building rapport as another positive experience. They felt that, compared with in-person consultations which are often highly time-pressured in China, telemedicine would allow more time with the patient. Whilst this contradicts findings from Western countries such as the US, telemedicine meetings in China often take place out of regular office hours, so the physician is able to give the patient more time, resulting in more empathy, emotional support and an improved patient-physician relationship. For this purpose, video-based models were considered most suitable (as opposed to text or phone call only).
“Telemedicine consultation takes place during the doctor’s spare time. The doctor is able to give the patient all their attention, so the doctor is more relaxed, and the patient becomes more relaxed. The doctor is able to empathize and see things from the patient’s perspective, as they are able to take the perspective of wanting to resolve the patient’s anxiety and take a more personal approach. It’s advantage [telemedicine] is more about being able to give emotional support to the patient and establish rapport.” (ECP, China)
On the other hand, telemedicine appears to have perceived limitations when it comes to diagnosing patients. Aside from the physical tests that diagnoses in ophthalmology often require, respondents expressed concerns about reaching an accurate diagnosis through virtual consultations only. Physicians felt they are too reliant on patient feedback that might not be accurate or sufficient, in particular, when it comes to complex conditions and the need to look at individual symptoms. Physicians expressed additional concerns about liability if a wrong diagnosis was reached, meaning physicians would only ever provide a recommendation and never a final diagnosis via telemedicine as a precautionary measure. Patients would always be asked to come into hospital for an in-person consultation and examination to confirm a final diagnosis. This lack of trust would need to be overcome before physicians and patients would feel comfortable using telemedicine as a diagnostic tool.
3. User-friendly interface and usability
Access to telemedicine tools should be facilitated by a seamless user experience. Specific needs or demographics of the target group such as age, technological proficiency to dexterity and physical ability need to be addressed.
In a recent blog about digital health in Asia, we explained how some healthcare mobile apps are targeting the silver surfer generation. To make their app more user-friendly and patient-centric, they have made changes to their interface, such as using a larger font size and more contrasting colors as well as giving the ability to connect family members.
In ophthalmology, patients often suffer from limited eyesight. The patients in our study proposed that a voiceover functionality where instructions and content are read out would be more appropriate than having to read text.
4. An acceptable price point
Finally, we discussed pricing options of telemedicine services from the patient’s perspective. Our research found that in China, a consultation at the hospital with a specialist costs RMB40 (US$6). In comparison, a telemedicine app might charge between RMB 50-150 for a general doctor, which can rise significantly to RMB 1,000 (US$150) for a video consultation with a department head-level consultant. Many patients found that the price for a telemedicine consultation does not always justify the convenience benefit, particularly as virtual consultations sometimes do not deliver the same level of outcome as in-person visits. There were concerns that the physicians might still request the patient to come to the hospital after a telemedicine consultation, meaning they would have spent vast sums of money without actually benefitting from the telemedicine service.
“If I decide to do a telemedicine consultation because I’m drawn to the convenience or I don’t want to step out of my house, then just choosing the visual-text option already costs twice the amount I’ll pay for a hospital consultation with a specialist, and how much feedback can it give me?” (Ophthalmology patient, China)
Price can be a considerable barrier that needs to be considered in order to maximize uptake.
Conclusion
Telemedicine offers clear benefits in terms of convenience. However, services must demonstrate that they are effective in saving customers time and money, and also that they facilitate access to care by offering relevant services along the entire patient journey. It will be vital for anyone developing a tool to engage with the target group to better understand their needs and desired outcomes to ensure the telemedicine solution supports patient centricity and engagement.
At Research Partnership, we have conducted multiple studies evaluating telemedicine services across a range of therapy areas. If you would like to find out more about how our experts can help you achieve maximum success with a telemedicine solution, please contact us now and we will get back to you with further information.
Find out more about our experience conducting research in emerging markets